Abstract
BACKGROUND Acute pulmonary embolism (PE) is a common, potentially life-threatening disease. It is estimated that 5-15% of patients with acute PE are at high risk of death or hemodynamic collapse. Multiple risk stratification models have been developed to identify patients at risk of complications. Common examples include, simplified Pulmonary Embolism Severity Index (sPESI) and Hestia criteria scores. The sPESI has demonstrated the ability to discriminate between high (score ≥ 1) and low risk (score =0) for 30-day mortality. Hestia criteria (score ≥ 1 = high risk, score = 0 low risk) has shown ability to identify low risk patients eligible for outpatient treatment. However, neither scoring model takes into account the presence of right ventricular dysfunction (RVD), a predictor of early mortality. Our objective was to compare the ability of 4 different risk stratification models to identify outpatients at risk of mortality up to 90 days after acute PE
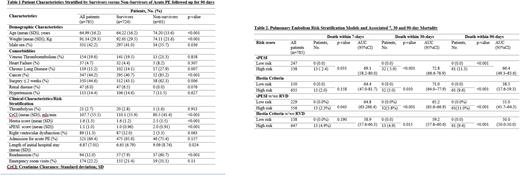
METHODS We conducted a retrospective cohort study of adult outpatients aged ≥18 years with objectively confirmed PE from 2014-2019. PE was identified by positive diagnostic imaging from radiology reports obtained via search of the Picture Archiving and Communication System (PACS) database in Eastern Health Region in Newfoundland and Labrador, Canada. Patient data was collected via manual chart review. We calculated sPESI and Hestia scores for each patient with confirmed PE using methods from original derivation studies. Patients were stratified into 4 categories according to sPESI or Hestia criteria alone, as well as a combination of sPESI or Hestia criteria with or without (w/wo) RVD. High risk PE included those with sPESI or Hestia = 0 with RVD. Categorical data are presented as percentages and continuous data are shown as mean±SD. Students t-test and X2 test were used to compare continuous and nominal variables, respectively. The Cox regression analysis was used to analyse all-cause mortality up to 90 days in each category. Area under the receiver operator curve was used to measure the discrimination of each of the 4 risk stratification models to estimate 7, 30 and 90-day mortality (AUC). AUC: 50%, 50-69%, ≥70-80%, >80-90% and >90-100% suggest no, modest, acceptable, excellent and outstanding discrimination respectively.
RESULTS A total of 785 outpatients were included in this study and had a mean [SD] age of 64.9 [16.2] years; weight, 91.1 [29.4] kg; and 331 were male [42.2%]). About 17.6-31.5% were classified as low risk by the 4 risk stratification models. Death rate at 7, 30 and 90 days ranged from 2.4-11.3%, 2.0 - 9.6%, 2.3 - 11.0%, 4.9 - 9.4% for patients categorized by sPESI, Hestia criteria, sPESI w/wo RVD and Hestia w/wo RVD respectively in the high risk groups. No death occurred in low risk groups. Of the 4 models, sPESI and Hestia showed acceptable discrimination for 30-day mortality with AUC: 72.8 (95%CI; 66.6-78.9) and 71.0 (95%CI; 64.0-77.9) respectively. This suggests sPESI score and Hestia criteria have a 72.8% and 71.0% chance of properly identifying low-risk and high-risk individuals based on 30-day mortality risk, respectively. Use of sPESI alone demonstrated modest discrimination for risk of 7 [AUC; 69.1 (95%CI; 58.2-80.0)] and 90-day [AUC; 66.4 (95%CI; 49.3-83.6)] mortality while Hestia criteria alone showed modest discrimination for risk of 7-day mortality [AUC: 64.4 (95%CI: 47.0-81.7)] but poor discrimination for 90-day risk of mortality [AUC; 38.5 (95%CI: 17.6-59.3)]. Each risk stratification model discriminated modestly for 7-day mortality (AUC range, 58.9-69.1), with sPESI showing the highest and Hestia w/wo RVD the least. In each model, discrimination for 90-day was lowest (AUC range, 38.5-66.4) compared to 7 and 30-day mortality. Hestia w/wo RVD exhibited the least discrimination for risk of mortality (AUC; 50.0-59.2).
CONCLUSION: Compared to other risk models, sPESI alone showed acceptable discrimination at identifying acute PE patients at risk of 30-day death and modest discrimination at 7 and 90 days and performed better across the three time trajectories. Use of Hestia criteria alone showed acceptable and modest discrimination at identifying patients at risk of 30 and 7-day death respectively but least discrimination for 90-day mortality compared to sPESI w/wo RVD and Hestia w/wo RVD. The Hestia w/wo RVD model had the least discrimination at identifying risk of 7 and 30-day mortality compared with other models.
Disclosures
Bonsu:Sanofi Canada: Research Funding. Young:Sanofi Canada: Research Funding; Bayer Canada: Research Funding; Pfizer: Honoraria. Lee:Shoppers Drug Mart: Research Funding. Chitsike:Sanofi Canada: Research Funding; Bayer Canada: Research Funding; Pfizer: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal